
As part of its global efforts to prepare for future pandemics, the MUSICC consortium has initiated collaborations with two leading biobanks in the Netherlands via its partners – the Leiden Medical University Center (LUMC) Central Biobank Facility and the Erasmus Medical Center (Erasmus MC) Central Biobank . Through these partnerships, MUSICC has introduced protocols to improve the safety and viability of the samples stored in their biobanks. These samples will play a critical role in facilitating MUSICC’s scientists to develop coronavirus challenge agents for use in the project’s future human challenge studies.
Patient samples are scarce material, stored in very small amounts and cannot necessarily be provided to other parties due to limits of consent. However, the new protocols introduced, as part of the Dutch biobanks’ collaboration with MUSICC, will also streamline access for authorised researchers. One such example is the sharing of the isolated virus, that would contain no personal patient data.
Accessing challenge agents for research has sometimes been difficult in the past, as biobanks in various locations hold different virus strains and it cannot be certain what will be gathered from patients . But with the successful collaboration of the LUMC and Erasmus MC Central Biobanks with MUSICC, the project will have the necessary challenge agents ready to move onto the next round of human challenge trials.
Biobanks are quietly transforming the way we approach medical research. They can be thought of as libraries of biological samples and provide scientists with some of the base materials needed for understanding diseases and developing treatments. One such potential treatment are mucosal vaccines that could stop viruses from infecting people in the first place and so limiting viral spread.
Laying the groundwork for these vaccines is a key part of MUSICC’s work and it intends to do this through the use of human challenge studies . To do this, MUSICC scientists need access to stocks of specific virus strains. This is where the biobanks at LUMC and Erasmus MC come in.
Both biobanks store samples of respiratory viruses and coronaviruses, held as blood and nasal swab samples. A range of viruses are stored, such as human coronaviruses (HCoVs) OC43 and 229E which are mostly known for the common cold, but also samples of the SARS-CoV-2 virus which causes COVID-19.
At LUMC, samples of this virus are stored within the Leiden University Centre Infectious Disease (LUCID) Biobank which forms part of the LUMC Central Biobank Facility. The LUCID biobank was set up in 2020, with the first additions being SARS-CoV-2 samples collected during the COVID-19 pandemic.
The Erasmus MC Central Biobank was also built in 2020 and stores samples across 64 freezers at -80°C. All these biobanks serve many research projects and outputs, and their supply of respiratory virus and coronavirus samples have now made them a valuable part of MUSICC.

Storage freezers at the Erasmus MC Central Biobank store samples at -80°C. Credit: Erasmus MC
Since these biobanks handle samples containing potentially infectious pathogens, safety and biosecurity are extremely important. The facilities are highly regulated, and laboratory workers there follow strict protocols to ensure safe and secure storage, access and processing of samples, and safe destruction of all waste from the labs. Staff working in the facility are highly trained for up to a year before they can even begin working with the samples, which are safely locked in a vault with restricted access.
Samples are collected from patients, residing in the biobank’s respective institution hospitals, initially to conduct diagnostics but they are also of high value for various kinds of research. Patients must give permission for samples to be taken from them for the biobanks, and they are given clear information on how their samples will be used.
Once collected, the samples are catalogued alongside anonymised medical data which provides context about the patient’s medical status at the time of collection. These samples can then be used to create suitable challenge agents for use in MUSICC’s human challenge studies.
The collaboration between MUSICC and the biobanks is already showing positive impacts on evolving biobank practices. Previously, patient nasal samples for the Dutch biobanks were collected as a single nasal swab, but this can prove challenging and risky for developing challenge agents due to factors such as contamination and logistical constraints. Following collaboration with MUSICC, the biobanks now collect two nasal swabs from each patient to create the best scenario for challenge agent development.
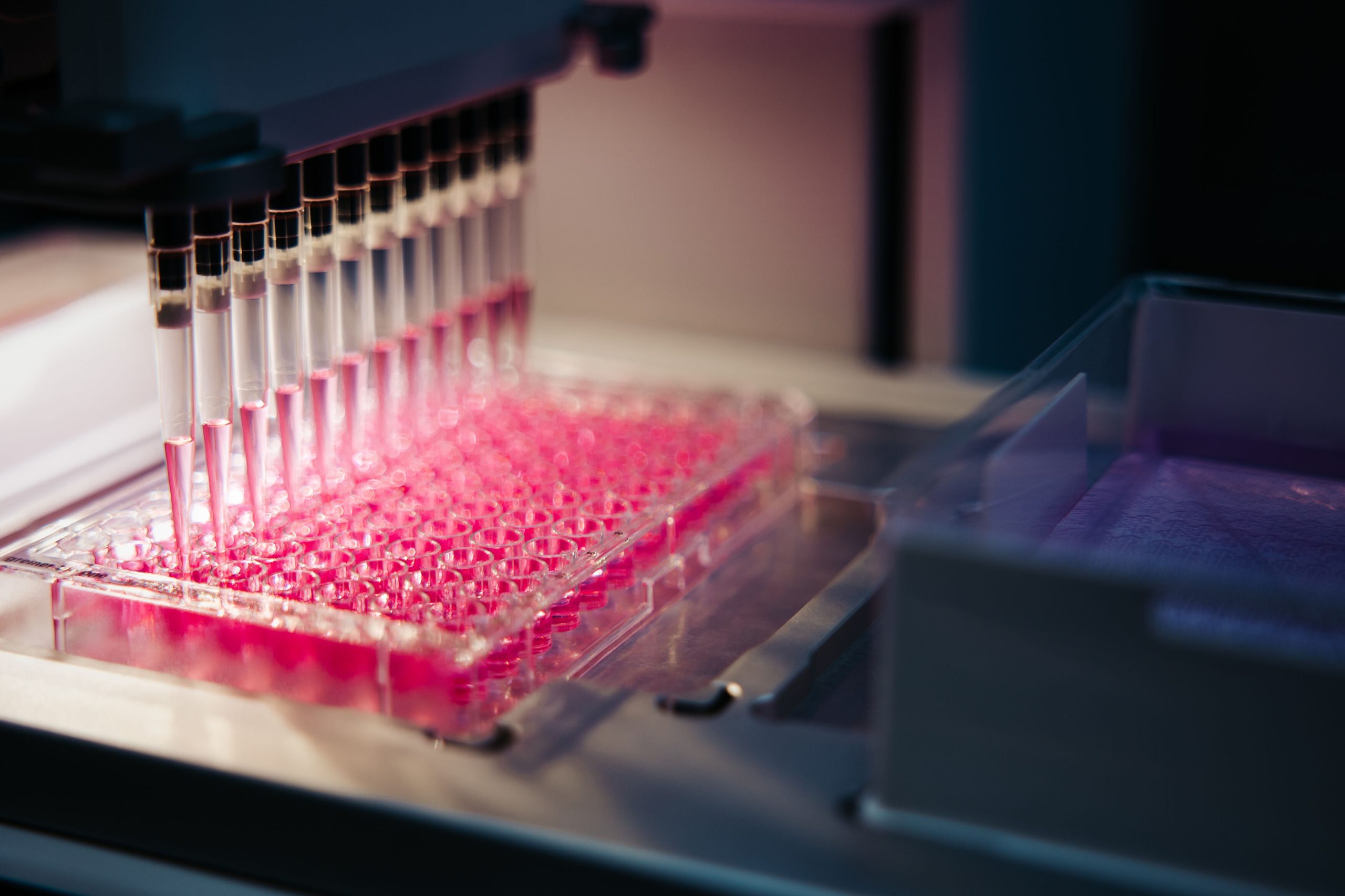
Processing of biological samples. Credit: LUMC
To develop challenge agents for MUSICC, the genetic data of a designated virus will be copied from the virus within a patient sample. Before the viral genetic data can be copied the first patient sample needs to be defrosted and then the virus within the sample needs to be analysed to ensure it is suitable for challenge agent development. Suitability criteria for the virus include the correct genetic make-up, no other pathogens (or co-infections) present in the sample, and a sufficient amount of the virus present.
These criteria are vital in developing safe and high-quality challenge agents. Determining the amount of virus present in a sample ensures only samples with sufficient viral content are selected and scientists do this using a technique called quantitative polymerase chain reaction (qPCR).
The presence of additional pathogens in coronavirus patient samples can provide useful data to help understand possible common co-infections with coronaviruses. However, samples with co-infections are not used to develop challenge agents as this would put human challenge study volunteers at unnecessary risk.
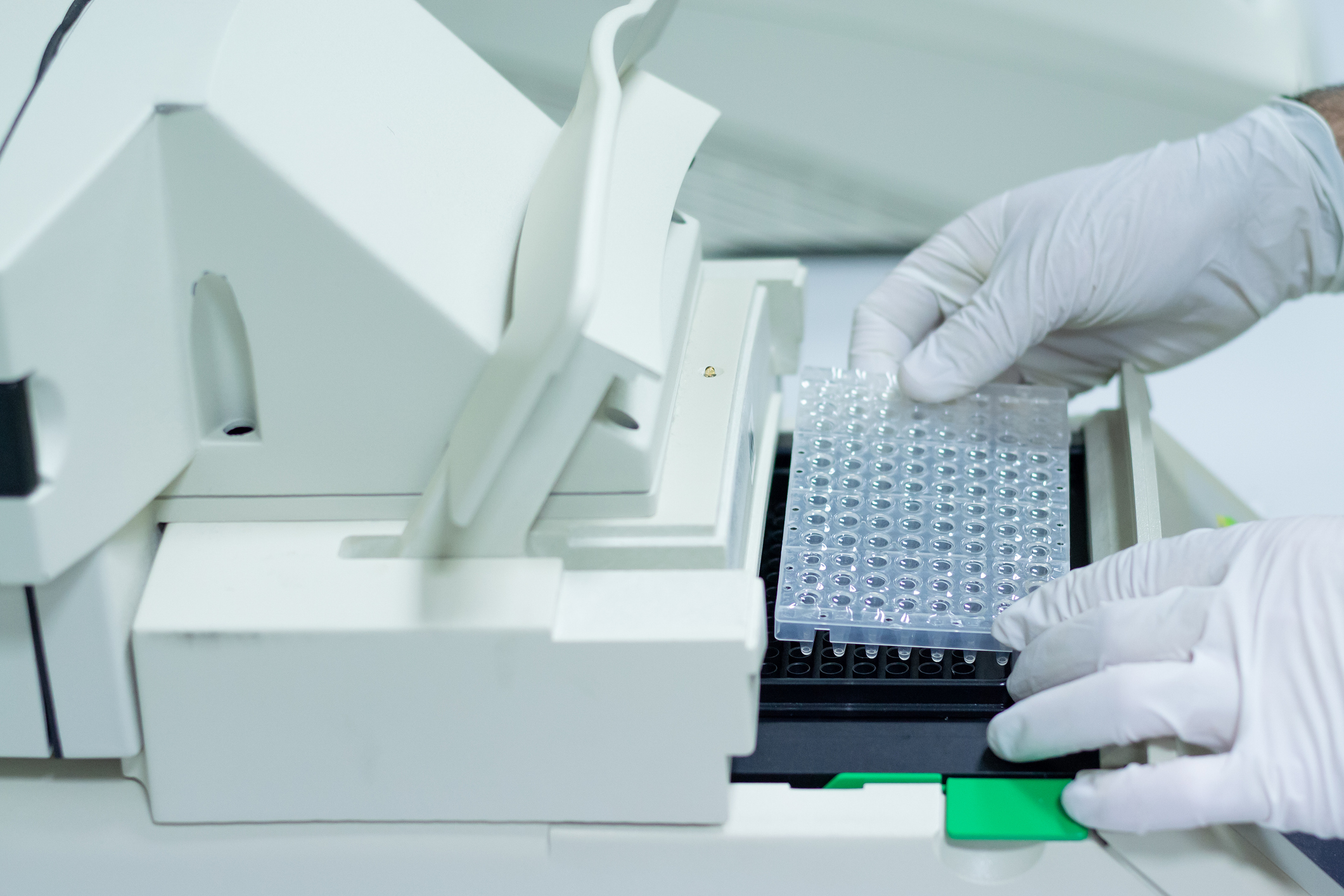
Samples being loaded into a qPCR machine. Credit: Oscar Martinez Troncoso\iStock via Getty Images
If a sample proves to be viable for developing a challenge agent, MUSICC’s scientists can then return to the biobank and use the second, still frozen sample from the same patient. Unlike the first sample, the second sample is defrosted in a Good Manufacturing Practice (GMP) lab – a lab that follows strict quality standards.
It is not feasible to defrost and analyse all the first samples in the GMP lab due to logistical and time constraints and transferring them to a GMP lab after defrosting would carry other challenges and risks, such as possible contamination. The protocols around developing GMP-grade virus stocks is a key part of the work for MUSICC partners LUMC and Erasmus MC, as detailed in our recent article about their work.
Once the second sample is defrosted, scientists can then isolate and copy the genetic material of the virus within. This means that only the virus, and no biological material of the patient, is carried forward to develop the challenge agent.

Staff must wear a range of personal protective equipment when working with the viral samples depending on the level of risk identified. Credit: LUMC
One of MUSICC’s goals is to facilitate the quick and efficient set up of future human challenge studies in order to accelerate vaccine testing, while still retaining the same high-level of safety as previous longer studies. The biobanks and the work of the teams involved are key components to the success of this mission.
“Biobanks are the cornerstone of modern biomedical research, laying the foundation for breakthroughs across a broad spectrum of scientific challenges—including the development of complex and novel agents. The CEPI co-funded MUSICC initiative has meaningfully accelerated this effort by expanding access to well-characterized respiratory samples and refining their application in controlled human infection model (CHIM) studies. This paves the way for transformative research that will resonate far beyond its original scope and intent, encompassing health challenges well beyond its original remit.”
Dr Jutte de Vries – Clinical Virologist, Associate Professor and LUCID Biobank founder.
MUSICC’s mission is for the impact of this work to resonate far beyond the reaches of this consortium and advance research innovation in human challenge studies and pandemic. If successful, this will advance research not only for coronaviruses, but potentially any pathogen with pandemic potential.

18th December 2025